When blood calcium levels begin to drop below homeostatic levels, it can trigger a cascade of physiological consequences. This article delves into the intricacies of calcium homeostasis, exploring the factors that lead to hypocalcemia, its impact on bodily systems, and the clinical strategies employed to manage this condition.
Calcium, an essential mineral, plays a pivotal role in maintaining skeletal integrity, facilitating neuromuscular function, and regulating hormonal balance. Its levels in the body are tightly regulated through a complex interplay of hormones, dietary intake, and renal function.
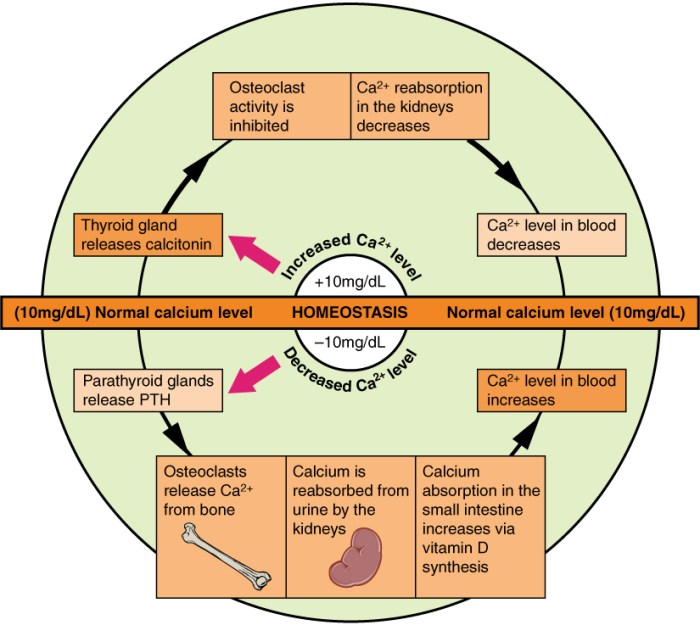
Calcium Homeostasis and Regulation
Calcium plays a pivotal role in maintaining various physiological functions, including neuromuscular transmission, bone health, and cellular signaling. To ensure optimal functioning, the body employs intricate mechanisms to regulate calcium levels within a narrow range.
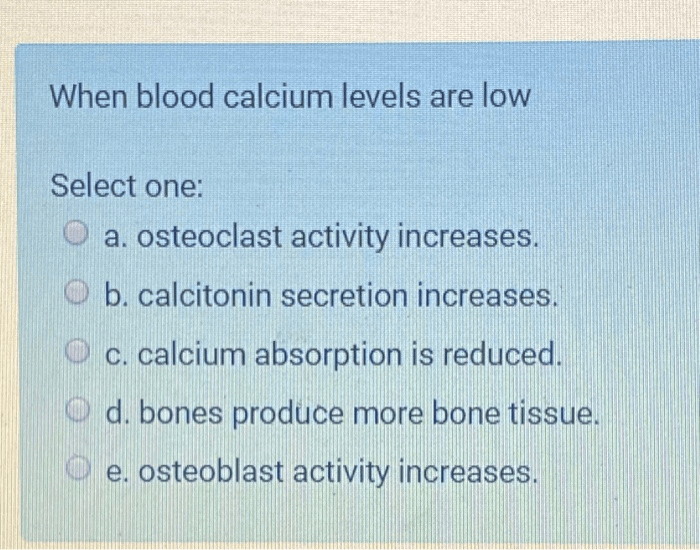
The primary hormone involved in calcium homeostasis is parathyroid hormone (PTH), secreted by the parathyroid glands. PTH acts on bones and kidneys to increase calcium reabsorption and decrease excretion, respectively. Conversely, calcitonin, a hormone produced by the thyroid gland, promotes calcium deposition in bones.
Vitamin D, a nutrient obtained through diet and sunlight exposure, facilitates calcium absorption from the intestine.
Causes of Hypocalcemia, When blood calcium levels begin to drop below homeostatic levels
Hypocalcemia, a condition characterized by low blood calcium levels, can result from various factors:
- Nutritional deficiencies:Inadequate dietary intake of calcium or vitamin D can lead to decreased calcium absorption.
- Hormonal imbalances:Deficiencies in PTH or excessive calcitonin production can impair calcium regulation.
- Medical conditions:Hypoparathyroidism, kidney failure, and pancreatitis can disrupt calcium homeostasis.
Specific disorders associated with hypocalcemia include rickets, osteomalacia, and tetany.
Consequences of Hypocalcemia
Low blood calcium levels can have profound physiological consequences:
- Neuromuscular dysfunction:Hypocalcemia can cause muscle weakness, cramps, and seizures due to impaired nerve transmission.
- Bone health:Calcium is essential for bone formation and maintenance. Hypocalcemia can lead to bone loss, osteoporosis, and increased fracture risk.
- Other systemic effects:Hypocalcemia can also affect the heart, kidneys, and skin, leading to arrhythmias, kidney stones, and dry skin.
Symptoms of hypocalcemia may include paresthesias, muscle cramps, fatigue, and mood changes.
Clinical Management of Hypocalcemia
Diagnosing hypocalcemia involves measuring blood calcium levels and assessing the underlying cause.
Treatment strategies aim to restore calcium levels and address the underlying etiology:
- Calcium supplementation:Oral or intravenous calcium supplements can be administered to increase blood calcium levels.
- Hormone replacement therapy:In cases of PTH deficiency, PTH injections may be prescribed.
- Dietary modifications:Increasing dietary calcium intake and ensuring adequate vitamin D levels can help prevent and manage hypocalcemia.
The following table summarizes the differential diagnosis and management options for hypocalcemia:
| Condition | Cause | Diagnosis | Treatment |
|---|---|---|---|
| Primary hypoparathyroidism | PTH deficiency | Low blood calcium, elevated PTH | PTH injections |
| Pseudohypoparathyroidism | PTH resistance | Low blood calcium, normal or elevated PTH | Calcium and vitamin D supplements |
| Vitamin D deficiency | Inadequate vitamin D intake | Low blood calcium, low vitamin D levels | Vitamin D supplements |
| Renal failure | Impaired calcium reabsorption | Low blood calcium, high phosphorus levels | Calcium supplements, phosphate binders |
Essential FAQs: When Blood Calcium Levels Begin To Drop Below Homeostatic Levels
What are the common causes of hypocalcemia?
Nutritional deficiencies (vitamin D, calcium), hormonal imbalances (parathyroid hormone), and certain medical conditions (renal failure, pancreatitis) can all contribute to decreased blood calcium levels.
How does hypocalcemia affect the body?
Low blood calcium levels can lead to neuromuscular irritability, bone demineralization, impaired cognitive function, and arrhythmias.
What are the treatment options for hypocalcemia?
Treatment typically involves calcium supplementation, hormone replacement therapy (parathyroid hormone or vitamin D), and dietary modifications to increase calcium intake.